ejection : 방출, 분출,배출
fraction : 부분, 일부
exertion : 노력, 분투
aneurysm : 동맥류
dangling : ~에게 결과를 알리지 않고 기다리게 하다, ~을 애타게 (안달복달하게 )하다
Ray-naud's phenomenon : 손가락 끝 부분의 조직이 혈액 내 산소부족으로 손상돼 색조변화, 통증, 조직괴사 등을 가져오는 질환.
belching : 트림
indigestion : 소화불량(증)
diaphoresis : 발한
intensive : 집중적인, 철두철미한, 많은 주의를 기울여 하는
look into : 조사하다, ~의 속을 들여다보다, 주의깊게 살피다
dislodgement : 제거, 강제로 이전시킴
interpretation : 해석, 이해, 설명
proceed : 진행하다, 나아가다,계속해서 -을 하다 ( = go on )
metformin : "비구아니드" 계열의 경구용 혈당강하제로서 식이요법, 운동 요법과 병행하여 제2형 당뇨병에 사용
asymptomatic : 증상이 없는
causative : 원인이 되는
vigorous : 활발한, 격렬한
herbal product ( eg.Ginkgo biloba ) : 허브로만든 물품? ( eg. 은행나무 )
Ointment ( eg. Vit.E ) : 연고
incision : 절개
prolapse : 탈출 ( 증 )
occasional : 가끔의
substernal : 복장밑, 흉골하
precipitate : (특히 나쁜 일을 )촉발시키다, (갑자기 어떤 상태로) 치닫게 하다
intercourse : 교류
exposure : (유해한 환경 등에의) 노출, 폭로, (언론을 통해)알려짐,다뤄짐
friction : 마찰
unilateral : 일방적의, 단독의
prominent : 중요한, 유명한
varicose vein : 정맥류성 정맥
scrotum : 음낭
abdominal girth : 복부둘레
appetite loss : 식욕부진
thrombosis : 혈전증
diminished : 감소된, 권위가 떨어진
diminish : 줄어들다, 약해지다, 줄어들다, 약화시키다
안압 정상수치 : 10-21 mmHg
mucous : 점액선(샘)
exertional : 운동성의
dyspenic : 호흡 곤란의
occasional : 가끔의
hypertrophy : ( 인체장기, 조직 등의 ) 비대
ejection : 분출, 배출
eject : 쫒아내다, 내쫒다
consistent : 한결같은, 일관된
crackle : 수포음
disseminated : 파종성의, 산재성의
coagulation : 응고, 응고물
specify : (구체적으로 ) 명시하다
improving :개량하는, 유익한, 도움되는
Unilateral : 일방적인, 단독의
Occasional : 가끔의
contraction : 수축, 축소, 진통
congestion : 혼잡,울혈, 충혈/울혈/점액에의한 막힘
admit : 인정[시인]하다, 자백하다, 들어가게 하다, 입장을 허락하다
clammy skin : 냉습피부
clammy : (기분 나쁘게) 축축한
potent : (힘이) 센[강항]
rehebillitation : 재활치료
contribute to : ~에 기여하다
further : 추가의, 더 이상의, (거리상) 더 멀리에
every other day : 이틀에 한번
prioritized : 우선순위를 매기다
---
air hunger : 공기 기아 ( 심장병/천식에서 기인한 ) 호흡곤란
frothy : 거품이 떠 있는
stridor : 천명 ( 호흡기관의 협착이 원인 ) , [문이 ] 삐걱거리는 소리
diffuse : 널리 퍼진, 분산된
lung periphery : 폐 주변부
strenuous : 힘이 많이 드는, 몹시 힘든, 격렬한.
restriction : 제한, 제약, (자유를 )구속하는 것
strengthen : 강화되다, 강력해지다, 강화하다
elderly client : 나이든 고객
foul smelling : 악취가 나는
scaly skin : 비늘 모양의 피부
presence : (특정한 곳에)있음, 존재(함), 참석
absence : 결석, 결근, 부재
tibial : 경골의
claudication : 파행, 절뚝거림
impaired : 손상된, 제 기능을 못하는
taut : 팽팽한, 긴장된
admitting : 인정하다, 시인하다
pharmacologic : 약리학의
instruction : 설명, 지시, 설명하는
intervention : 중재
rate : 속도, 평가하다, 평가되다, 좋다고 생각하다
diaphoretic : 발한성의
specimen : 견본, 샘플, 표본, 사료
impair : 손상[악화] 시키다
need to : ~을 할 필요가 있다.
indicate : 나타내다 [보여주다]
consent : 허락하다
verify : 확인하다
chest wall pain → pneumothorax 와의 감별을 위해 chest x-ray 우선촬영하기
obtain : 얻다, 존재하다
threaten : 협박/위협하다, (나쁜일이 있을) 조짐을 보이다, 위태롭게 하다
threatened : ( 야생동물의 종이) 멸종위기에 처한
verbalize : 말로 표현하다
indication : (사정,생각,감정을 보여주는 ) 말[암시/조짐]
indicate : (사실임/존재함을) 나타내다
hydrochorothiazide : 이뇨제,혈압강하제
lisinopril : ACE 억제제
clonidine : 혈관운동중추에 억제적으로 작용해서 혈압을 저하시키는 강압제.
nitroprusside sodium : 나이트로프루사이드 나트륨. 항고혈압제.
determine : 알아내다, 밝히다, 결정하다, 확정하다
abrupt : 돌연한, 갑작스러운
adherence : 고수
adherence to : ~에의 집착(고수)
bruit : (소식 등을 ) 유포하다
stethoscope : 청진기
diapragm : 횡격막
outpouching : 팽출, 외번, 낭상돌출
swishing : 휙[쌩] 소리를 내며 움직이다
buzzing : 윙윙거리는, 와글와글 거리는
malaise : ( 특정 상황, 집단 내에 존재하는 설명, 규명하기 힘든 ) 문제들 [불안감]
advanced : 선진의, 고읍의, 후기의
pursed-lip breathing : 입술 오므리기 호흡
visceral : 강한 감정에 따른, 내장의
perietal pericardium : 벽쪽 심장막
inspiration : 영감
Inspire : 고무[격려]하다, 영감을 주다 , { 감정 등을 } 불어넣다 [ 고취시키다]
friction : 마찰
distinguish : 구별하다, 구별짓다, 식별하다
simvastatin : 지질저하제로서 혈중의 콜레스테롤 생성을 감소시킵니다.
prop : 지주, 받치다, 소품
noticed : 신경씀, 주목, 알아챔
nail beds : 손발톱바닥, 조상, 손톱밑바닥
presence : (특정한 곳에) 있음, 존재(함), 참석
throbbing : 고통치는, 요동치는
antacid : 제산제
progression : (한 단계·상태에서 다음 단계·상태로의 점진적인) 진행[진전]
administering : 관리하다, 집행하다
anticipate : 예상하다
rehabilitation : 재활치료
abstain : 자제하다
subcutanous : 피하의
absent : 없는, 부재한
palpate : 촉진하다
atypical : 이례적인
indigestion : 소화불량(증)
intensive : 집중적인
altered : 바뀐
endothelial : 내피의
hypercoagulability : 응고항진성
captopril : 안지오텐신 변환효소저해제의 항고 혈압약. 화학구조는 안지오텐신과 유사하고 효소 저해로 인해 혈관수축성의 안지오텐신II의 생성이 감소한다. 전구체 안지오텐신I에는 혈관확장작용이 있으므로 II의 감소와 함께 강압작용이 나타난다. 혈소판응집억제 작용도 있다. 고레닌성 고혈압증에 사용
spironolactone : 스피로노락톤은 특히 고알도스테론증이 중요한 역할을하는것으로 보이는 간경화 환자에게나 부종 치료제로 널리쓰이는 알도스테론 수용체 길항제와 칼륨 보존 이뇨제이다.
carvedilol : 카르베딜롤은 고혈압과 협심증에 사용되는 약물이다. 교감신경 수용체를 차단하여 혈관 저항성을 감소시킴으로써 혈압을 낮추고 협심증의 증상을 완화
enalapril : 고혈압 치료제
aggregation : cohesion 분자나 이온, 원자 등이 분자 사이의 힘이나 쿨롱인력의 작용으로 모이는 것.
strain : 부담, 중력, 압
thereby : 그렇게 함으로써, 그것 때문에
statin : 혈관 내 콜레스테롤 억제제
accumulater : (서서히 )모으다, 축적하다, 늘어나다[모이다]
typically : 일반적으로
define : 정의하다, 규정짓다
atherosclerosis : 동맥경화
complication : 문제, 합병증
calf : 종아리
immobilization : 부동, 고정시킴
popliteal : 오금의
groin : 서혜부, 사타구니
subjective : 주관적인
objective : 객관적인, 목적, 목표
fraction : 부분, 일부
thready : 실같은, 가느다란
detect : 발견하다
postural : (앉거나 서있는 ) 자세의
blowing : (공기, 증기의) 분출하는 소리
bigeminy : 이단현상, 이단맥
claudication : 파행
intermittent : 간헐적인
sublingual : 혀 밑의
consent : 동의
accompany : 동반하다, 수반하다
prophylactic : 예방의
prosthetic : 인공의
admitted to : ~의 입장을 허락하다. ~에 입원하다
nocturnal : 야행성의
paroxysmal : 발작성의
pedal edema : dependent of leg edema

| Distinguishing acid reflux from angina | ||
| GERD | Angina | |
| Symptoms |
|
|
| Symptom duration |
|
|
| Precipitating factors |
|
|
| Alleviating factors |
|
|
| ACS = acute coronary syndrome; GERD = gastroesophageal reflux disease. | ||
* Indicated interventions following coronary artery bypass grafting (CABG) include: Notifying the health care provider (HCP) of chest tube drainage >100 mL/hr, which could indicate hemorrhage.

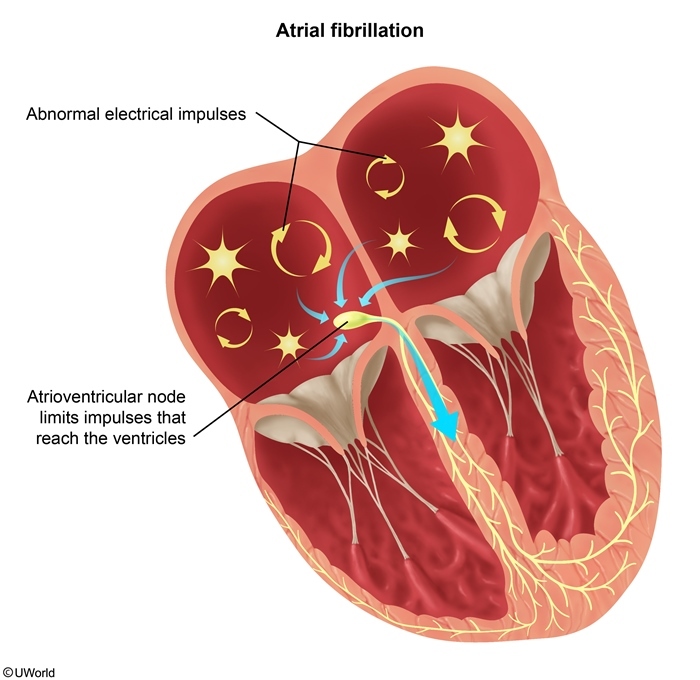
Atrial fibrillation (AF) is a common cardiac dysrhythmia that occurs following coronary artery bypass grafting (CABG). AF is characterized by the absence of P waves, presence of fibrillatory waves, and an irregularly irregular rhythm. Ineffective atrial contractions result in incomplete atrial emptying, decreased cardiac output, and increased risk for atrial thrombi formation due to blood stasis.
Clients with AF require antiarrhythmic medications (eg, beta blockers, digoxin) to control the ventricular rate and/or electrical cardioversion to convert the rhythm.
* Following CABG, clients are at risk for bleeding and fluid accumulation within the pericardial sac (ie, pericardial effusion). Hypotension may indicate progression to life-threatening hemorrhage or cardiac tamponade.
* Indicated interventions following coronary artery bypass grafting (CABG) include: Notifying the health care provider (HCP) of chest tube drainage >100 mL/hr, which could indicate hemorrhage.
* Clients with AF require antiarrhythmic medications (eg, beta blockers, digoxin) to control the ventricular rate and/or electrical cardioversion to convert the rhythm. -> amiodarone은 beta blocker
* AAA post OP : Pulses can be absent for 4-12 hours after surgery due to vasospasm. However, a pedal pulse decreased from the client's baseline or an absent pulse with a painful, cool, or mottled extremity 2 days postoperative can indicate the presence of an arterial or graft occlusion.
* Subcutaneous emphysema is air in the tissue surrounding the chest tube insertion site and can occur in a client with a pneumothorax. The nurse should assess lung sounds and palpate to determine the degree of emphysema. However, this is an expected finding, so the nurse does not need to assess this client first.
* The nurse needs to provide education to the client with a venous leg ulcer who refuses to wear compression stockings. Compression is essential for the treatment of chronic venous insufficiency, venous ulcer healing, and prevention of ulcer recurrence. The client will need individual evaluation to determine what level of compression is needed.
| Client teaching for heart failure | |
| Weight monitoring |
|
| Diet |
|
| Medication regimen |
|
| Activity |
|
| Symptoms to report |
|
Myocardial infarctions (MIs) damage heart muscle and require medications to improve heart function and prevent reinfarction (eg, aspirin). Aspirin, an antiplatelet agent, inhibits platelet aggregation, prevents thrombus formation, and reduces heart inflammation. Clients without signs of bleeding or low platelet levels may safely receive aspirin (Option 1).
Atorvastatin is a lipid-lowering medication given to clients to lower cholesterol levels (ie, LDL cholesterol), which reduces plaque and reinfarction risk (Option 2). However, statins may cause rhabdomyolysis and require monitoring for muscle weakness and pain.
Docusate sodium is a stool softener that reduces straining during bowel movements, thereby decreasing the workload on the heart. Straining can also cause bradycardia due to vagal response (Option 3).
Lisinopril is an ACE inhibitor often prescribed to clients after an MI to prevent ventricular remodeling and progression of heart failure. Lisinopril may cause hyperkalemia and hypotension, and should be administered only to clients with normokalemia and normotension (Option 4).
(Option 5) Metoprolol is a beta blocker prescribed to clients after MI to reduce the risk of reinfarction and heart failure. Metoprolol lowers blood pressure and heart rate; therefore, the nurse should hold the medication and notify the health care provider of hypotension or a heart rate <50/min.
* Cardiac catheterization involves injection of IV iodinated contrast to assess for obstructed coronary arteries.
Potential complications of IV iodinated contrast include:
- Allergic reaction: Clients with a previous allergic reaction to iodinated contrast may require premedication (eg, corticosteroids, antihistamines) to prevent reaction or an alternative contrast medium (Option 2).
- Lactic acidosis: When administered to clients taking metformin, IV iodinated contrast can cause an accumulation of metformin in the bloodstream, which can result in lactic acidosis. Therefore, health care providers may discontinue metformin 24-48 hours before administration of contrast and restart the medication after 48 hours, when stable renal function is confirmed (Option 4).
- Contrast-induced nephropathy: Iodinated contrast can cause acute kidney injury in clients with renal impairment (eg, serum creatinine >1.3 mg/dL [115 µmol/L]). Therefore, clients with renal impairment should not receive iodinated contrast unless absolutely necessary
* Angina pectoris is defined as chest pain brought on by myocardial ischemia (decreased blood flow to the heart muscle).
- Physical exertion (eg, exercise, sexual activity): Increases heart rate and reduces diastole (time of maximum blood flow to the myocardium)
- Intense emotion (eg, anxiety, fear): Initiates the sympathetic nervous system and increases cardiac workload
- Temperature extremes: Usually cold exposure and hypothermia (vasoconstriction); occasionally hyperthermia (vasodilation and blood pooling)
- Tobacco use and second-hand smoke inhalation: Replaces oxygen with carbon monoxide; nicotine causes vasoconstriction and catecholamine release
- Stimulants (eg, cocaine, amphetamines): Increase heart rate and cause vasoconstriction
- Coronary artery narrowing (eg, atherosclerosis 동맥경화, coronary artery spasm 경련 ): Decreases blood flow to myocardium
Acute pericarditis is inflammation of the membranous sac (pericardium) surrounding the exterior of the heart, which can cause an increase in the amount of fluid in the pericardium (ie, pericardial effusion). Increased pericardial fluid places pressure on the heart, which impairs the heart's ability to contract and eject blood. This complication (ie, cardiac tamponade) is life-threatening without immediate intervention.

Deep venous thrombosis (DVT) is a major concern in clients with unilateral leg pain after prolonged immobilization (eg, air travel, surgery) or those with obesity, pregnancy, or other hypercoagulable states (eg, cancer). Eighty percent of DVTs start in the veins of the calf and move into the popliteal and femoral veins. Classic symptoms include unilateral leg edema, local warmth, erythema, and low-grade fever. Therefore, the swelling in one leg is highly concerning.
* Discharge teaching for the client with a permanent pacemaker should include the following: should not perform shoulder range-of-motoin exercise,,
until approved by the HCP as this can cause dislodgement of the pacemaker lead wires.

Abdominal aortic aneurysms are surgically repaired when they measure about 6 cm or are causing symptoms.
Repair of abdominal aortic aneurysms can be done via femoral percutaneous placement of a stent graft (endovascular aneurysm repair) or via an open surgical incision of the aneurysm and placement of a synthetic graft. With either procedure, postoperative monitoring for graft leakage or separation is a priority. Manifestations of graft leakage include ecchymosis of the groin, penis, scrotum, or perineum; increased abdominal girth; tachycardia; weak or absent peripheral pulses; decreasing hematocrit and hemoglobin; increased pain in the pelvis, back, or groin; and decreased urinary output
The client must be monitored postoperatively for graft leakage and hemodynamic stability. Adequate blood pressure is necessary to maintain graft patency, and prolonged hypotension can lead to the formation of graft thrombosis. Signs of graft leakage include a decreasing blood pressure and increasing pulse rate.

Aortic stenosis is a narrowing of the aortic valve, which obstructs blood flow from the left ventricle to the aorta. As stenosis progresses, the heart cannot overcome the worsening obstruction, and ejects a smaller fraction of blood volume from the left ventricle during systole. This decreased ejection fraction results in a narrowed pulse pressure (ie, the difference between systolic and diastolic blood pressures) and weak, thready peripheral pulses. With exertion, the volume of blood that is pumped to the brain and other parts of the body is insufficient to meet metabolic demands, resulting in exertional dyspnea, anginal chest pain, and syncope.
* Orthostatic BP measurement may be done to detect volume depletion or postural hypotension caused by medications or autonomic dysfunction.
Procedure for measurement of orthostatic BP
- Have the client lie down for at least 5 minutes (Option 1)
- Measure BP and HR
- Have the client stand,,,
standing과 stand,, - Repeat BP and HR measurements after standing at 1- and 3-minute intervals (Option 4)
A drop in systolic BP of ≥20 mm Hg or in diastolic BP of ≥10 mm Hg, or experiencing lightheadedness or dizziness is considered abnormal (Option 2).
Educational objective:
To measure orthostatic BP, the nurse should have the client lie supine for 5-10 minutes and then measure BP and HR. The nurse should then have the client stand for 1 minute, measure BP and HR, and repeat the measurements at 3 minutes. Findings are significant if the systolic BP drops ≥20 mm Hg or the diastolic BP drops ≥10 mm Hg.

Murmurs are produced by turbulent blood flow across diseased or malformed cardiac valves. They can be characterized as musical, blowing, swooshing, or rasping sounds heard between normal heart sounds. The aortic area is located at the second intercostal space, right sternal border.

Ventricular paced rhythms are seen in clients with ventricular pacemakers. Ventricular pacemakers typically have one lead placed in the right ventricle. The pacer spike just before the QRS complex signals electrical stimulation of the ventricle by the pacemaker lead
* Acute-onset dyspnea and cough productive of pink, frothy sputum indicate severe pulmonary edema, likely a complication from myocardial infarction. Pink sputum results from ruptured bronchial veins due to high back pressure. The mix of blood and airway fluids creates the pink tinge. On assessment, crackles can be heard at the lung bases.

This client is exhibiting symptoms of intermittent claudication or ischemic muscle pain that can be due to peripheral artery disease (PAD). PAD impairs circulation to the client's extremities. The nurse should first check for the adequacy of blood flow to the lower extremities by palpating for the presence of posterior tibial and dorsalis pedis pulses and their quality. Poor circulation to the extremities can place the client at increased risk for development of arterial ulcers and infection.

Nitroglycerin sublingual to promote coronary artery vasodilation, increasing myocardial perfusion
* Complications of cardiac catheterization include bleeding, dysrhythmias, and stroke.
Nursing care after cardiac catheterization with percutaneous coronary intervention includes:
- Increasing fluid intake or IV fluids to promote clearance of IV contrast (Option 2).
- Keeping the affected leg straight for 2-6 hours as prescribed after femoral-approach cardiac catheterization; the head of the bed should remain at ≤30 degrees to prevent hip flexion that could disrupt clots at the insertion site and cause bleeding (Option 3).
- Providing antiplatelet therapy to reduce risk of blood clots because the stent is a foreign body that can cause platelet aggregation until a smooth surface is created. Aspirin is taken for life, and a P2Y12 receptor blocker (eg, clopidogrel) is taken for several months post-MI
* Hypertensive crisis is a life-threatening emergency due to the possibility of severe organ damage. If not treated promptly, complications such as intracranial hemorrhage, heart failure, myocardial infarction (MI), renal failure, aortic dissection, or retinopathy may occur.
Emergency treatment includes IV vasodilators such as nitroprusside sodium. It is important to lower the blood pressure slowly, as too rapid a drop may cause decreased perfusion to the brain, heart, and kidneys. This may result in stroke, renal failure, or MI. The initial goal is usually to decrease the MAP by no more than 25% or to maintain MAP at 110-115 mm Hg.
* client have COPD, HF,, how can nurse in determining if this is an exacerbation of HF?
-> B-type natriuretic peptide (BNP) is a peptide that causes natriuresis. BNPs are made, stored, and released primarily by the ventricles. They are produced in response to stretching of the ventricles due to the increased blood volume and higher levels of extracellular fluid (fluid overload) that accompany heart failure. Elevation of BNP >100 pg/mL (>28.9 pmol/L) helps to distinguish cardiac from respiratory causes of dyspnea
BNP는 증가된 혈액량( HF동반된)으로 심실의 Stretching 양에 따라 생산된다. 100 pg/mL 이상의 수치는 Cardiac으로부터 수반된 dyspnea를 구별하는데 도움을 준다..!!!

* Clients with peripheral arterial disease (PAD) have decreased sensations from nerve ischemia or coexisting diabetes mellitus. They should never apply direct heat to the extremity due to the risk for a burn wound. Wound healing is impaired in these clients.
Swelling in the extremities (edema) could result from venous stasis (venous valve incompetence or varicose veins); these clients are asked to elevate their extremities during rest. However, clients with PAD usually do not have swelling, but rather have decreased blood supply. The extremities should not be elevated above the level of the heart because extreme elevation further impedes arterial blood flow to the feet.
Additional teaching for the client with PAD includes the following:
- Smoking cessation
- Regular exercise
- Achieving or maintaining ideal body weight
- Low-sodium diet
- Tight glucose control in diabetics
- Tight blood pressure control
- Use of lipid management medications
- Use of antiplatelet medications
- Proper limb and foot care
* Certain individuals should receive prophylactic antibiotics prior to dental procedures to prevent infective endocarditis (IE). These include the following:
- Prosthetic heart valve or prosthetic material used to repair heart valve
* Abnormal heart tones: An S3 heart tone (eg, ventricular gallop) is characteristic of HF and occurs during early diastole when blood from the atria rapidly enters the ventricle and hits the less compliant (stiff) ventricular wall, creating an audible vibration.
* Heart failure (HF) is a chronic, progressive condition characterized by impaired ventricular function that leads to decreased cardiac output and causes blood to back up into the lungs and systemic circulation. An exacerbation of HF is identified by worsening symptoms, including:
- Crackles with auscultation and decreased capillary oxygen saturation: In clients with HF, blood backs up into the lungs (pulmonary edema) due to a failing left ventricle, producing crackles with auscultation and impairing alveolar gas exchange (Options 1 and 2).
- Elevated b-type natriuretic peptide (BNP): BNP is a hormone that produces natriuresis (ie, sodium elimination in urine) to compensate for fluid volume overload associated with HF. BNP is released in response to increased intraventricular volume and stretch (Option 3).
- Low left ventricular ejection fraction (EF) (ie, <50%): An echocardiogram is an ultrasound of the heart performed to view heart structures (eg, chambers, valves) and calculate EF. EF is a measure of the volume of blood pumped to the body from the left ventricle with each heart contraction. Low EF is caused by impaired ventricular function and represents worsening HF (Option 4).
- Lower extremity pitting edema: Peripheral edema is a sign of fluid volume overload that occurs in clients with HF when blood backs up into the venous circulation (Option 5).

* Pharmacologic management of heart failure (HF) focuses on reducing cardiac workload and improving cardiac output.
- Beta blockers (eg, carvedilol) reduce cardiac workload by inhibiting the action of catecholamines (eg, epinephrine, norepinephrine) on beta-adrenergic receptors in the heart. Beta blockers decrease myocardial oxygen demand by decreasing blood pressure and decreasing heart rate.
- Angiotensin-converting enzyme (ACE) inhibitors (eg, enalapril) alter the renin-angiotensin-aldosterone system by inhibiting conversion of angiotensin I to angiotensin II, thereby preventing the release of aldosterone. Aldosterone, an adrenal steroid hormone, retains sodium and water in addition to promoting vasoconstriction. By reducing circulating aldosterone, ACE inhibitors promote vasodilation and as a result decrease blood pressure. ACE inhibitors also decrease ventricular remodeling, an added benefit for clients with HF.
- Loop diuretics (eg, furosemide) prevent reabsorption of sodium and chloride in the kidneys, which increases urine output and fluid excretion. Decreases in circulating fluid volume will decrease blood pressure and reduce pulmonary edema (ie, increase oxygen saturation), as well as decrease cardiac preload.
* A troponin value of 0.7 ng/mL (0.7 mcg/L) indicates cardiac muscle damage and should be the priority and immediate focus of the nurse. Normal values: troponin I <0.5 ng/mL (<0.5 mcg/L); troponin T <0.1 ng/mL (<0.1 mcg/L).
* Sodium nitroprusside is a highly potent venous and arterial vasodilator.
* Client and family education is important for those with heart failure to prevent/minimize exacerbations, decrease symptoms, prevent target organ damage, and improve quality of life. The use of any nonsteroidal anti-inflammatory drugs (NSAIDS) is contraindicated as they contribute to sodium retention, and therefore fluid retention
* The client being admitted for heart failure-related fluid overload is likely to have dyspnea (difficulty breathing), orthopnea (labored breathing in a supine position), and paroxysmal nocturnal dyspnea (waking suddenly with difficulty breathing). The assessment phase of the nursing process must come before intervention and should be prioritized using the ABCs: airway, breathing, and circulation. Therefore, the nurse should first assess the client's breath sounds (Option 2). Rales or "crackles" may be auscultated in the lungs as a result of pulmonary congestion.
* Renal perfusion status is monitored closely in a client who has had abdominal aneurysm repair. Hypotension, dehydration, prolonged aortic clamping during surgery, blood loss, or embolization can lead to decreased renal perfusion and potential kidney injury. The nurse should routinely monitor the client's blood urea nitrogen (BUN) and creatinine levels as well as urine output. Urine output should be at least 30 mL/hr. This client should have an output of at least 120 mL of urine in a 4-hour period.
-> 만약 HF에 Urine output 30ml도 안나왔다? first action은 auscultate the client's breath sounds.
'NCLEX' 카테고리의 다른 글
| 5/6 cardiac, immune, visual/auditory (1) | 2023.06.09 |
|---|---|
| Chapter 68: Psychiatric Medications (2) (0) | 2023.04.17 |
| Chapter 68: Psychiatric Medications (1) (0) | 2023.04.16 |
| Chapter 67: Crisis Theory and Intervention (0) | 2023.04.15 |
| Chapter 66: Addictions (0) | 2023.04.14 |




댓글